UK Hot Weather Health Plan (Society for Acute Medicine)
The article below is an abridged version of the original text, which can be downloaded from the right-hand column. Please access the original text for more detail, research purposes, full references, or to quote text.
The Society for Acute Medicine has produced the following guidance to support clinicians working in acute services to:
- Work safely during hot weather conditions.
- Know who is at risk and adapt individual care plans to respond to hot weather.
- Be aware of medications that increase patient risk during hot weather.
- Know how to treat heat related illnesses including increased cardiovascular and respiratory complications.
- Be familiarised with the advice from public health to share with patients.
- Promote environmental and behavioural changes that could reduce the risk of hot
weather.
Hot weather mitigation and adaptation
Heatwaves in the UK have become more frequent, with soaring hospital temperatures and infrastructure ill-prepared to cope—up to 90% of NHS buildings are prone to overheating.
In the Evaluation of the Heatwave Plan for England’s 2019 national survey many frontline staff were unaware of any local heatwave plans and unfamiliar with the Heatwave Plan for England guidance. Few or none of the staff surveyed were able to enact the recommended Heatwave Plan actions during an alert. In December 2024 the UK government published guidance for healthcare professionals to reduce the risks of hot weather to their patients in the community, care homes and hospital environments. This included a brief statement regarding medication storage and the risk to staff.
Working Conditions (for staff and facility management)
Employers have a legal duty to ensure workplaces are maintained at a reasonable
temperature and the working environment is safe. There is no legal maximum temperature
for workplaces, as this will vary according to the work environment; however, employers
must be aware of the UK heat-health alert system [8] and have in place an appropriate
heatwave plan or guidelines to keep staff safe and well in hot weather.
The document (downloadable from the right-hand side) provides guidance for staff and facility management, some of which include:
- Keep everyone hydrated with water or juice.
- Reduce indoor heat by shutting off heat-generating devices.
- Control ventilation: close windows during hotter hours and open during cooler periods.
- Use fans only when temperatures stay under about 35 °C.
- Relocate especially vulnerable patients to cooler rooms (ideally under 26 °C).
- Advise light, breathable clothing; encourage cooling measures like showers or dampening clothes.
- Promote civility among staff and patients, since heat may heighten irritability.
Advice for patients include:
- Avoid peak sun (11 am–3 pm); wear sunscreen and reapply often.
- Discourage alcohol, or encourage alternating with water.
- Avoid storing medications in hot spots (e.g., cars, window sills).
- Limit sun exposure to around 20 minutes if outdoors.
- Emphasize fluid intake, loose clothing, and checking in on vulnerable individuals (e.g., elderly, isolated).
Weather Alerts (Heat-Health Alert System)
Green to Red alert levels outline escalating impacts:
- Green: minimal health effects.
- Yellow & Amber: rising mortality and healthcare demand; hospital environments may overheat.
- Red: widespread health risks, workforce strain, infrastructure breakdowns, increased heat-related illnesses.
Vulnerable Populations
Groups at heightened heat risk include:
- Older adults, individuals with chronic illnesses (e.g., cardiovascular, respiratory, neurological), disabilities, mental health conditions, pregnant women, young children, outdoor workers, the homeless, socially isolated individuals.
- Heat combined with air pollution increases respiratory/cardiac risks, and dehydration raises infection/sepsis risk (especially among older adults).
Medications Review during Heatwaves
Key actions to protect patients on medications during heat:
- Maintain drug storage under 25 °C; monitor utility room and fridge temperatures.
- Note medication adjustments or precautions in discharge summaries.
- Medications to review include:
- Electrolyte-altering meds (e.g., ACE inhibitors, diuretics, NSAIDs, SGLT2 inhibitors, digoxin, lithium).
- Drugs affecting thermoregulation (e.g., antipsychotics, antidepressants, beta-blockers, anticholinergics, Parkinson’s drugs, stimulants, opioids).
- Photosensitive or transdermal drugs (e.g., doxycycline, amiodarone, fentanyl patches) that may be affected by heat or UV.
- Counsel patients on symptom awareness and consider temporary medication changes or hydration relaxation during hot days.
Health Complications of Extreme Heat Exposure
Common heat-related conditions and treatment advice:
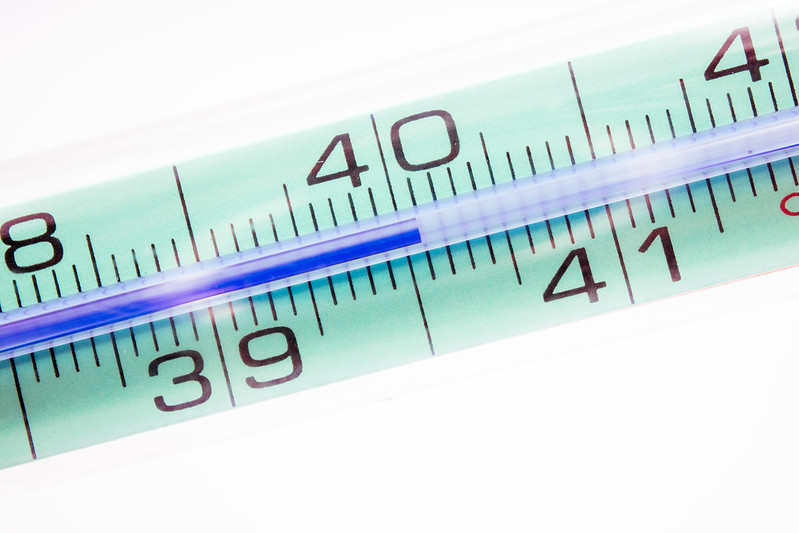
- Heat stroke: A medical emergency—body temp >40 °C, confusion, seizures, unconsciousness; treat with IV isotonic fluids, avoid antipyretics, and manage seizures per protocol.
- Sunburn / Heat rash: Use fluids, cool compresses, OTC analgesia/antihistamines; avoid occlusive creams; calamine ruled safe.
- Heat cramps: Encourage fluids and electrolyte replacement; usually self-resolving.
- Heat exhaustion: Watch for headache, fatigue, confusion, GI upset; manage with oral fluids, rest; escalate to emergency care if needed.
Differential Diagnosis
Important conditions to consider when evaluating hyperthermia:
- Toxicological causes (e.g., malignant hyperthermia, serotonin syndrome).
- Endocrine emergencies (e.g., thyrotoxicosis, adrenal crisis).
- Infections or central nervous system issues (e.g., sepsis, encephalitis)
- Distinguish based on history, symptoms, and lab findings.



Comments
There is no content